Introduction
Predictive Health AI is an advanced technological discipline that uses machine learning algorithms to analyze complex healthcare datasets and identify individuals at risk of developing conditions before symptoms appear. This article presents a clear, implementable framework for deploying Predictive Health AI, bridging the gap between theoretical models and real-world clinical impact.
Designed for healthcare technology strategists, clinical informaticians, and data science professionals, this guide explains how Predictive Health AI can transform proactive and preventive care.
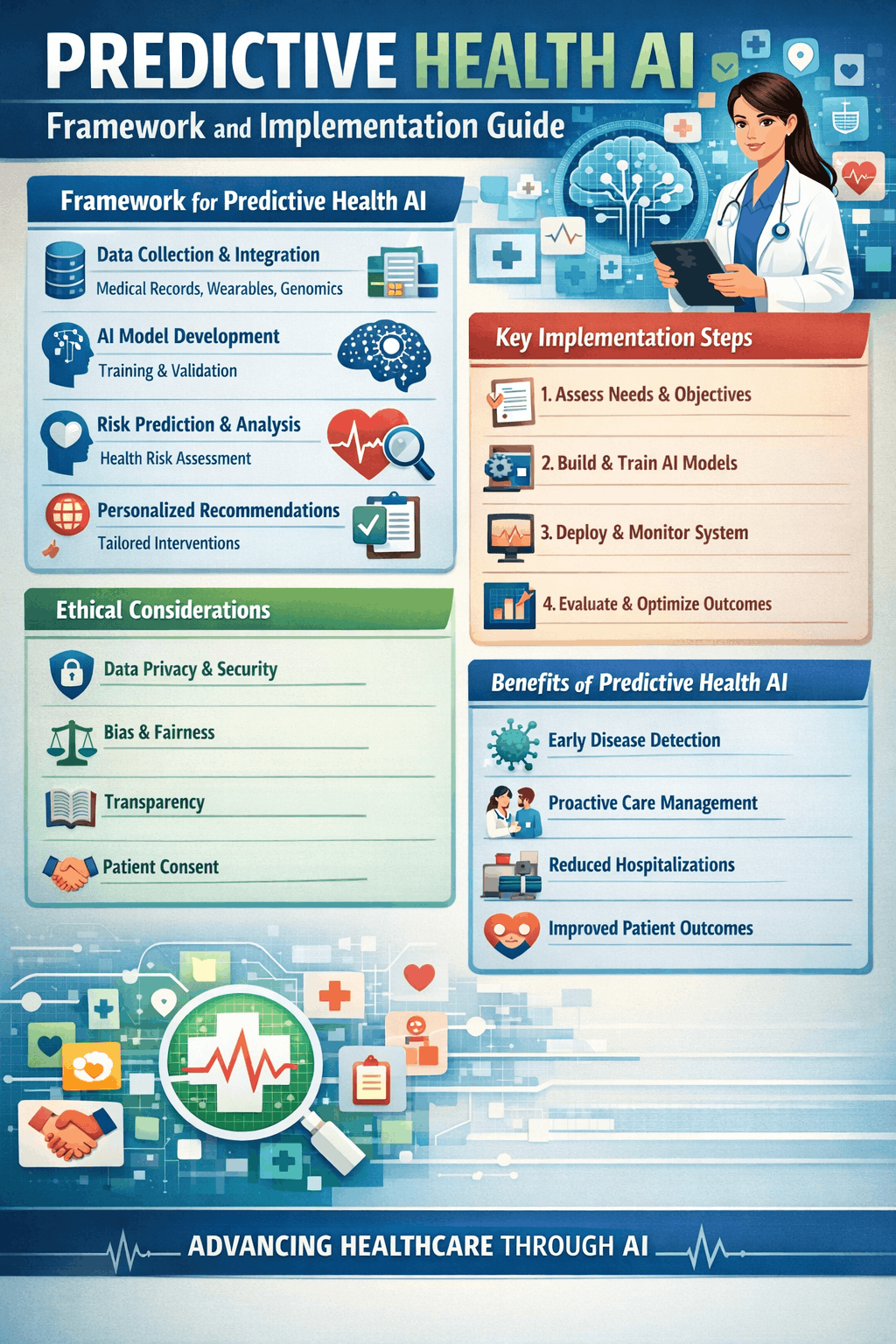
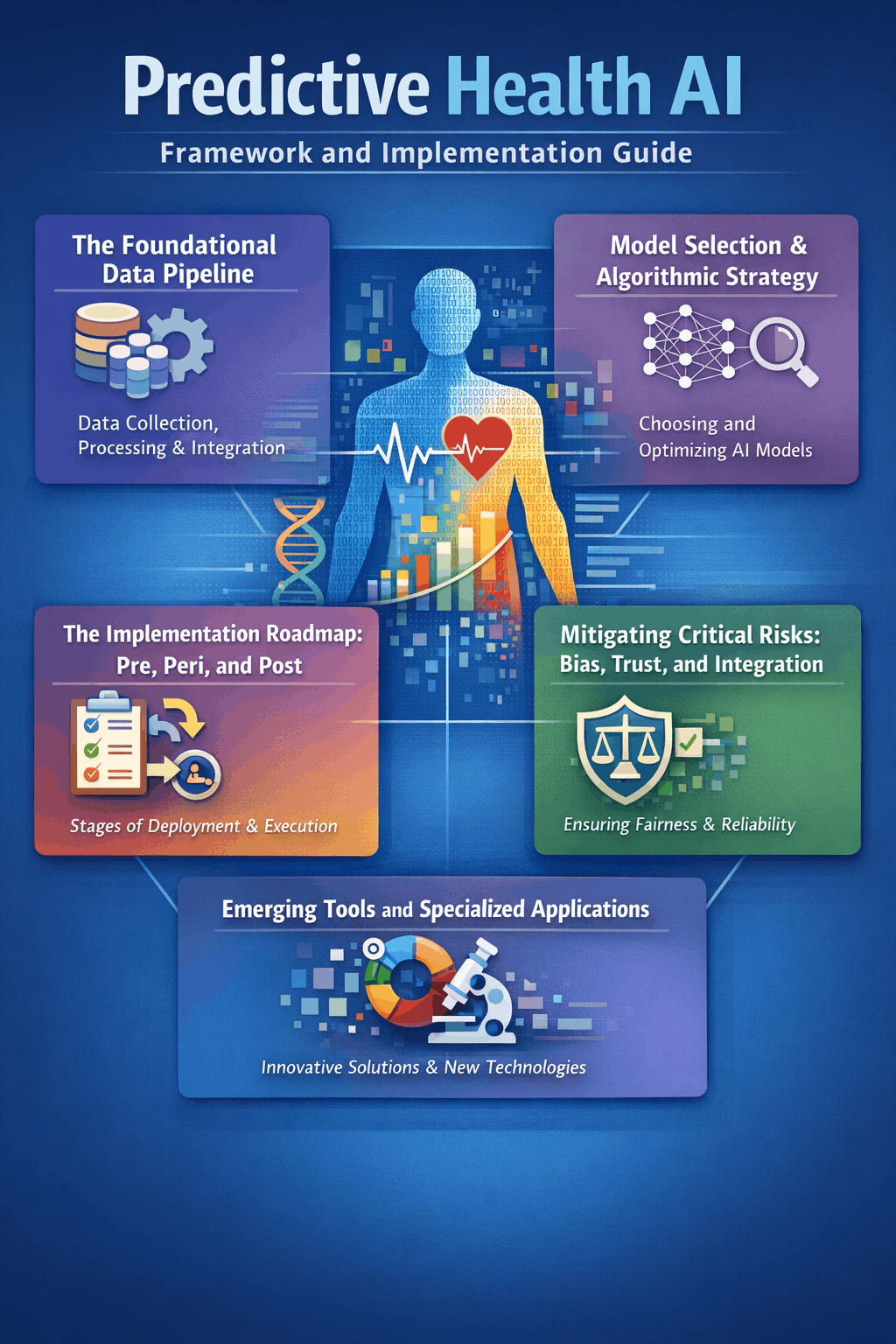
The Foundational Data Pipeline
Success begins with data quality and accessibility. A predictive model is only as reliable as the data it processes. The first technical pillar involves integrating multimodal data streams. This includes structured electronic health records (EHRs), diagnostic imaging, continuous readings from wearable devices, genomic data, and patient-reported outcomes. The primary challenge is overcoming fragmented “data silos” across different hospital systems, labs, and devices. Effective implementation requires a unified data platform, such as a Healthcare Intelligence Cloud, to normalize and consolidate these disparate sources into a single, analytics-ready data lake. Without this clean, structured foundation, predictive insights are unreliable.
Model Selection & Algorithmic Strategy
Model architecture is dictated by the clinical question and data type. The systematic review identifies clear patterns: tree-based ensemble models like Random Forest and XGBoost are most prevalent for structured, tabular EHR data due to their strong performance and relative interpretability. For complex, unstructured data like medical images or longitudinal time-series data (e.g., vital sign trends), deep learning architectures such as Convolutional Neural Networks (CNNs) and Long Short-Term Memory (LSTM) networks are more effective. The key is matching the tool to the task—use classification models for risk stratification (high/medium/low), regression models to predict continuous outcomes like length of stay, and clustering models to identify novel patient phenotypes.
The Implementation Roadmap: Pre, Peri, and Post
A peer-reviewed roadmap structures deployment into three critical phases, ensuring safety and efficacy.
- Pre-Implementation: Before live deployment, conduct exhaustive local validation. A model developed elsewhere may suffer from “dataset shift” and fail in your specific patient population. Rigorously evaluate performance using metrics beyond simple accuracy, including AUC, F1-score (for imbalanced data), and calibration. Crucially, map the clinical workflow and technical infrastructure. Determine how data will flow from the EHR to the model via APIs (e.g., FHIR standards) and how predictions will be delivered back to clinicians at the right time and in the right context.
- Peri-Implementation: Begin with a “silent pilot,” where the model runs in the background without alerting clinicians, to verify real-time data feeds and output stability. Follow this with a controlled, small-scale pilot in a single department. This phase tests user interfaces, measures clinician trust, and gathers feedback to refine alert mechanisms and prevent alert fatigue.
- Post-Implementation: Deployment is not the end. Establish a continuous monitoring and surveillance Model performance can decay due to changes in clinical practice, disease patterns, or data quality. Implement a governance structure for regular audits, model retraining protocols, and a clear decommissioning plan.
Measuring Real-World Impact and Success
The ultimate metric is not algorithmic performance but clinical and operational improvement. Define success based on tangible outcomes aligned with initial goals. This could be a reduction in 30-day hospital readmissions, earlier detection of sepsis leading to decreased mortality, more efficient allocation of nursing staff, or a reduction in clinician administrative burden. Tools like Decision Curve Analysis can help quantify the net benefit of the model’s predictions by balancing true positives against false positives in a clinical context.
Mitigating Critical Risks: Bias, Trust, and Integration
Ignoring these risks leads to project failure and potential harm.
- Algorithmic Bias & Equity: Proactively evaluate and mitigate bias at every phase. Assess model performance across demographic subgroups (race, gender, age) to ensure equitable accuracy. Scrutinize training data for representativeness and justify the inclusion of sensitive variables like race or socioeconomic status.
- Explainability & Clinician Trust: Black-box models pose a barrier to clinician trust and are therefore unlikely to be deployed in healthcare settings. Prioritize explainable AI (XAI) techniques to help clinicians understand the “why” behind a prediction. Trust is built through transparency about the model’s intended use, limitations, and confidence scores.
- Workflow Integration: The AI must fit seamlessly into existing clinician routines. Clunky integrations that add extra clicks or time will be abandoned. Adhere to the “Five Rights” of clinical decision support: delivering the right information, to the right person, in the right format, through the right channel, at the right time.
Emerging Tools and Specialized Applications
The landscape features powerful, specialized tools:
- AI-Powered Analytics Platforms: Solutions like Innovaccer and SAS Viya offer healthcare-specific environments for building, validating, and deploying predictive models with built-in governance.
- Specialized Clinical AI: Tools like Aidoc provide real-time, FDA-cleared AI for radiology, flagging urgent findings in CT scans and X-rays.
- Generative AI Integration: LLMs are moving beyond administration to clinical reasoning. Models like DeepSeek-R1 and specialized suites like Hippocratic AI’s Polaris 3.0 are designed for safe patient interaction and clinical support, though they require rigorous evaluation for predictive tasks.
- Expanding Domains: Robust applications are proven in mental health, where AI conversational agents can significantly reduce symptoms of anxiety and depression, and in chronic disease management, where predictive analytics enable personalized prevention plans.
Final Synthesis: From Pilot to System of Intelligence
Predictive Health AI transitions healthcare from a reactive to a proactive discipline. The journey from a successful pilot to a scalable system of intelligence requires treating AI not as a one-time project but as core, continuously managed infrastructure. This demands ongoing investment in data governance, clinician partnership, and ethical oversight. The organizations that succeed will be those that master the integration of advanced technology with unwavering focus on human-centric outcomes, equitable care, and sustainable workflow change.
FAQs
What is the first step in starting a predictive health AI project?
The first step is to define a specific, measurable clinical or operational problem (e.g., reduce heart failure readmissions by 15%), not to select an algorithm.
How long does it take to implement a predictive AI model in a hospital?
From initial scoping to full integration, expect a timeline of 12-24 months, accounting for data preparation, validation, piloting, and phased rollout.
Can predictive AI replace doctors?
No. Its role is to augment clinical judgment by providing data-driven insights and prioritizing attention, with the final decision always resting with the human clinician.